Conquering Chronic Obstructive Pulmonary Disease (COPD)
COPD does not imply “Coughing and Puffing Disorder”! It refers to a chronic lung condition whose hallmark is obstructed airways. COPD or Chronic obstructive pulmonary disease is a disorder in which subsets of patients may have dominant features of chronic bronchitis, emphysema, or asthma. The result is irreversible airflow obstruction.
Definition Of COPD
Chronic bronchitis is defined clinically as the presence of a chronic productive cough for 3 months during each of 2 consecutive years. Emphysema, on the other hand, is defined pathologically as an abnormal, permanent enlargement of the air spaces distal to the terminal bronchioles.
Airflow limitation in emphysema is due to loss of elastic recoil, whereas chronic bronchitis leads to narrowing of airway caliber. Although some patients predominantly display signs of one or the other, most fall somewhere in the middle of the spectrum.
Prevalance Of COPD
The exact prevalence of Chronic Obstructive Pulmonary Disease in the United States, as in the rest of the world, is unknown. This is largely due to the fact that it is an under diagnosed (and undertreated) disease.
The most recent study estimates a prevalence of 10.1% in the United States. COPD is the fourth leading cause of death in the United States. Currently the rates in men are higher than the rates in women.
Clinical Features Of Chronic Obstructive Pulmonary Disease (COPD)
Most patients with COPD have smoked at least 20 cigarettes per day for 20 or more years. Common symptoms include cough, sputum, and dyspnoea presenting in the fifth decade of life. The cough is productive, usually worse in the mornings and produces a small amount of colorless sputum. Breathlessness is the most significant symptom, but it usually does not occur until the sixth decade of life. Wheezing may occur in some patients, particularly during exertion and exacerbations. Systemic manifestations comprise decreased fat-free mass, impaired systemic muscle function, osteoporosis, anemia, depression, pulmonary hypertension, cor pulmonale, and even left-sided heart failure.
Patients with severe disease experience tachypnea (increased respiratory rate) and respiratory distress with simple activities. Use of accessory respiratory muscles and paradoxical indrawing of lower intercostal (between ribs) spaces is evident (known as the Hoover sign). In advanced disease, cyanosis, elevated jugular venous pulse (JVP), and peripheral edema are observed. Thoracic examination reveals hyperinflation (barrel chest), wheezing, diffusely decreased breath sounds, hyperresonance on percussion, and prolonged expiration. Coarse crackles beginning with inspiration may be heard, and wheezes frequently are heard on forced and unforced expiration.
Causes Of COPD
Cigarette Smoking
Clinically significant Chronic Obstructive Pulmonary Disease develops in 15% of cigarette smokers.Age of initiation of smoking, total pack-years, and current smoking status predict COPD mortality.
Air Pollution
Although the role of air pollution in the etiology of COPD is unclear, the effect is small when compared with cigarette smoking.
Airway Hyperresponsiveness
Individuals who have nonspecific airway hyperreactivity and who smoke are at increased risk of developing COPD.
Alpha1-Antitrypsin Deficiency
AAT deficiency is the only known genetic risk factor for developing COPD and accounts for less than 1% of all cases in the United States. Severe AAT deficiency leads to premature emphysema at the average age of 53 years for nonsmokers and 40 years for smokers.
Treatment Of COPD
Smoking Cessation
The goal of management is to improve the quality of life by preventing symptoms and the recurrence of exacerbations. Smoking cessation continues to be the most important therapeutic intervention. The success rates of smoking cessation plans are low because of the addictive power of nicotine.
Smoking cessation involves behavioral counseling and nicotine replacement therapies. Nicotine polacrilex, a chewing gum, and Transdermal nicotine patches (NicoDerm, Nicotrol, and Habitrol) are alternatives.
Bronchodialtors
Inhaled delivery of medications is preferred over the oral route to help minimize potential adverse effects. Further, long-acting bronchodilators are more beneficial than short-acting ones.
Beta-Agonists
In Chronic Obstructive Pulmonary Disease COPD, beta2 agonists produce less bronchodilatation compared with asthma. Patients primarily use beta2 agonists for relief of symptoms of COPD. In patients with mild intermittent symptoms, it is recommended to use a short-acting beta2 agonist for symptomatic relief. In patients with more persistent symptoms, a long-acting beta agonist should be used.
Long-acting beta agonists have been shown to increase exercise endurance, prevent nocturnal dyspnea, and improve quality of life. Inhaled Albuterol (also known as Salbutamol)(VENTOLIN/ACCUNEB/PROVENTIL) , Terbutaline(BRETHEAIRE) and Salmeterol (SEREVENT) are the popular drugs currently used. These are saliently combined with inhalational steroids such as Fluticasone or Beclomethasone for use in chronic asthmatics.
Anticholinergics
Anticholinergic drugs compete with acetylcholine for postganglionic muscarinic receptors, thereby inhibiting bronchomotor tone, resulting in bronchodilatation. They block vagally mediated reflex arcs that cause bronchoconstriction.
Short-acting anticholinergics such as Ipratropium(ATROVENT) bromide in patients with stable Chronic Obstructive Pulmonary Disease have been shown to have equivalent or superior activity when compared with a beta2 agonist. However, in combination with a beta2 agonist, synergistic effect on bronchodilatation occurs. This medication has slower onset and a longer duration than a beta2 agonist and is less suitable for use on an as-needed basis. Typically, Ipratropium (ATROVENT) bromide is administered 2 to 4 puffs every 6-8 hours.
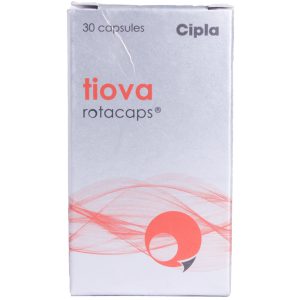
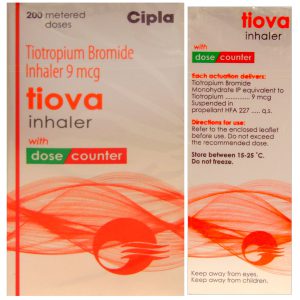
COPD Treatment Using Spiriva
Tiotropium (brand name Spiriva) is a once-daily, long-acting anticholinergic medication that has been shown to have significant clinical benefit and is a first-line therapy in patients with persistent symptoms.
Tiotropium (SPIRIVA) has a high level of bronchoselectivity and possesses minimal side effects if any via the inhalational route. Spiriva capsules are for use only in the Spiriva HandiHaler device.
Precautions when using Spiriva
The precautions when using Spirivainclude narrow-angle glaucoma, or an enlarged prostate or bladder obstruction. If you have any of these conditions, you may not be able to use tiotropium (SPIRIVA) inhalation or you may need a dosage adjustment or special tests during treatment.
SPIRIVA belongs to FDA pregnancy category C. It is not known whether tiotropium(SPIRIVA) inhalation is harmful to an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant during treatment. It is not known if tiotropium (SPIRIVA) passes into breast milk or if it could harm a nursing baby. Do not use tiotropium (SPIRIVA) inhalation without telling your doctor if you are breast-feeding a baby.
Phosphodiesterase Inhibitors
Adding theophylline (QUIBRON-T) to the combination of bronchodilators can result in further benefit in stable COPD patients. However, the narrow therapeutic index of theophylline has caused a decline in its popularity.
Patients metabolize theophylline primarily by the hepatic enzyme system, a process affected by age, the heart, and liver abnormalities. Serum levels of theophylline need to be monitored because of the potential for toxicity. Adverse effects include anxiety, tremors, insomnia, nausea, cardiac arrhythmia (particularly multifocal atrial tachycardia), and seizures. Hence, the previously recommended target range of 15-20 mg/dL has now been reduced to 8-13 mg/dL.
Oxygen Therapy
COPD is commonly associated with progressive hypoxemia. Oxygen administration reduces mortality rates in patients with advanced COPD because of the favorable effects on pulmonary hemodynamics.
Two landmark trials, the British Medical Research Counsel (MRC study) and the National Heart, Lung, Blood Institutes Nocturnal Oxygen Therapy Trial (NOTT), showed that long-term oxygen therapy improves survival 2-fold or more in hypoxemic patients with Chronic Obstructive Pulmonary Disease.
Chronic Obstructive Pulmonary Disease Treatment – Conclusion
Ever heard this one “To stop smoking is the easiest thing I ever did. I ought to know because I”ve done it a thousand times”!
Well you’ve got to make it (quitting) last as well as your last (cigarette), or else you won’t last! I mean, we need to have some inhaling capacity left, for SPIRIVA to bathe our bronchi.